How To Get Immediate Relief For Sciatica Pain: 9 Easy Ways
If you’re dealing with sciatica pain, you know how debilitating it can be. The sharp, shooting pain down your leg can make it difficult to do even the simplest things, like getting out of bed or walking.
But don’t despair, there are a number of things you can do to get immediate relief for sciatica pain. In this blog post by Buynetmeds , we’ll share 9 easy tips that have been proven to work for many people with sciatica.
We’ll also talk about the causes of sciatica pain, who’s at risk, how to cure sciatica permanently, and when to see a doctor.
Let’s get started!
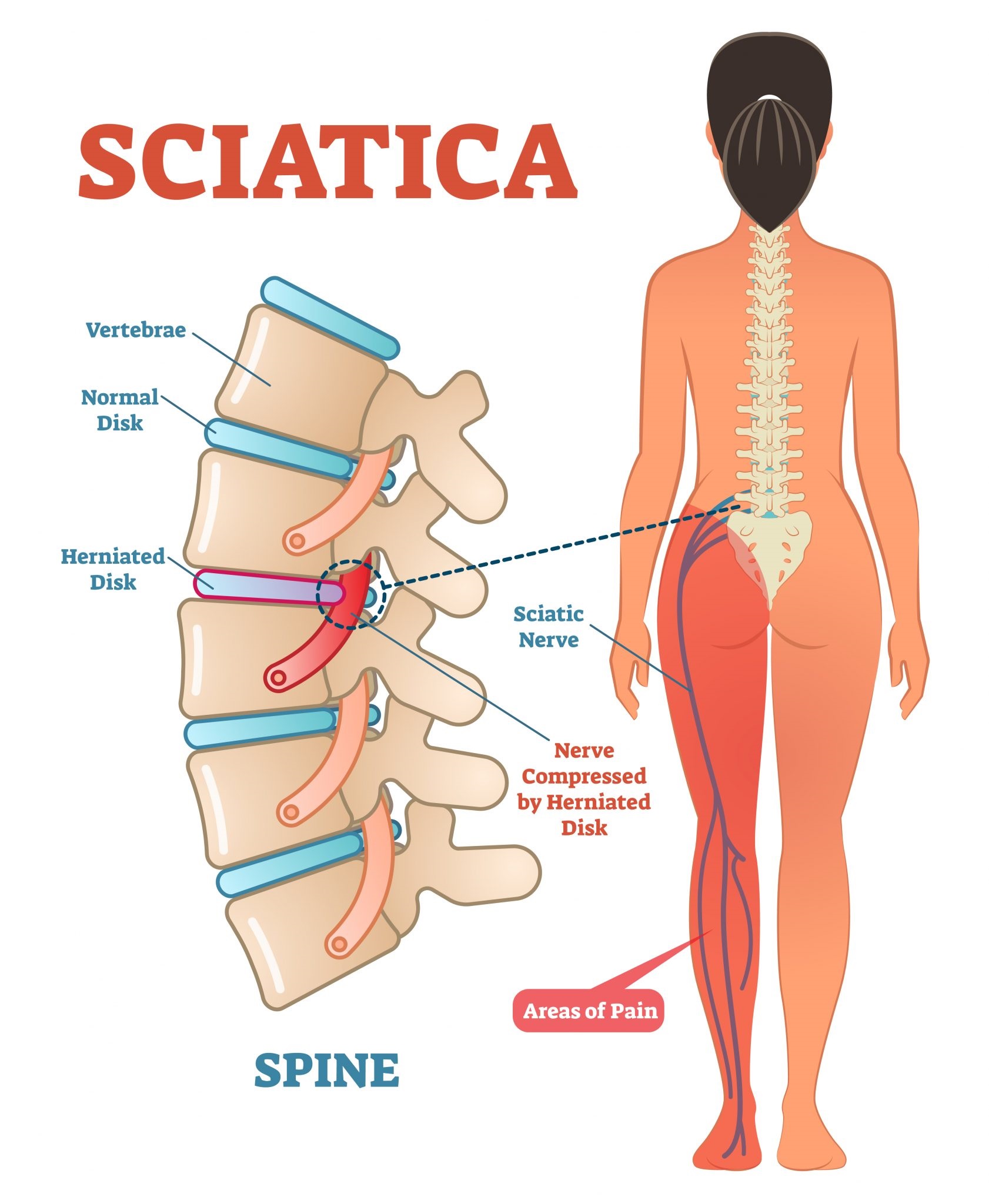
What is sciatica pain?
Sciatica is a type of pain that radiates along the path of the sciatic nerve, the longest nerve in the body. The sciatic nerve starts in the lower back and runs down through the buttocks and legs, ending in the feet. Sciatica pain can be mild or severe, and it can be constant or intermittent. It can also be accompanied by numbness, tingling, and weakness in the affected leg.
Sciatica pain is most common in adults between the ages of 30 and 50. However, it can occur at any age. People who are more likely to develop sciatica pain include:
- People who have jobs that require heavy lifting or bending
- People who are overweight or obese
- People who have diabetes
- People who have a family history of sciatica pain
What are the symptoms of sciatica pain?
Imagine a big, thick nerve running down your back and leg. That’s the sciatic nerve. If that nerve gets irritated or compressed, it can cause pain, numbness, and tingling in your leg. That’s sciatica.
The most common symptom of sciatica is pain down the back of one leg. The pain can be mild or severe, and it can be constant or intermittent.
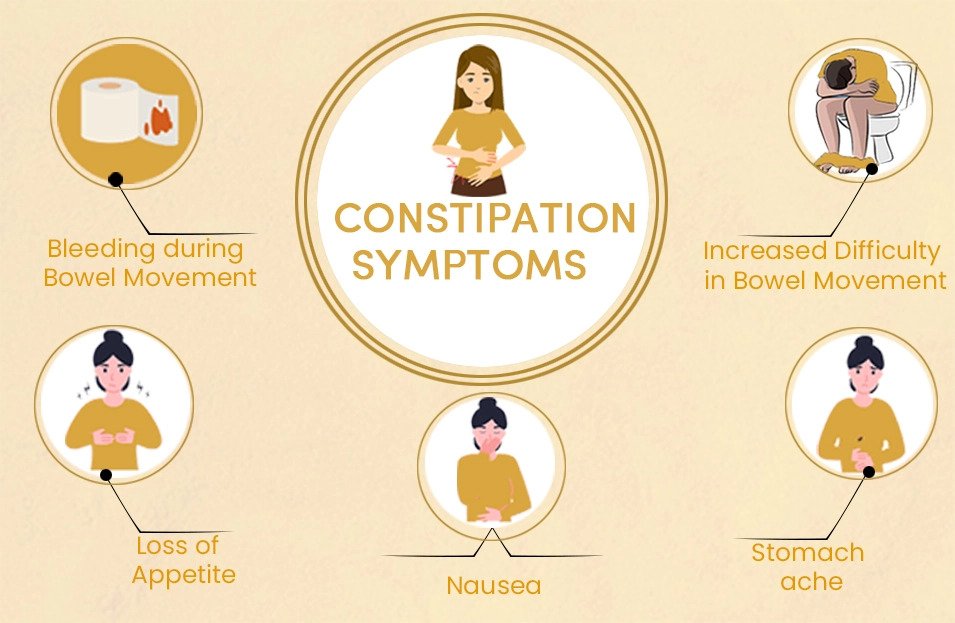
Other symptoms of sciatica pain may include:
- Pain in the lower back or buttocks
- Pain that worsens when sitting or standing
- Pain that worsens when coughing or sneezing
- Difficulty moving the affected leg
- Muscle weakness in the affected leg
- Numbness or tingling in the affected leg or foot
Sciatica pain is usually worse on one side of the body. However, it can affect both legs in some cases.
9 Easy Ways to Get Immediate Relief for Sciatica Pain

1. Rest:
When you have sciatica pain, it’s important to rest your back and avoid activities that make the pain worse. This may mean taking a few days off from work or avoiding certain activities like lifting heavy objects or exercising. Say goodbye to sciatic nerve pain in just 10 minutes with this natural method.
If you have to sit or stand for long periods of time, try to take breaks every 20-30 minutes to move around and stretch. You may also want to consider using a lumbar pillow or support cushion to help support your back.
2. Ice:
Ice can help to reduce inflammation and pain, so it’s a great way to get immediate sciatic nerve pain relief. Apply ice to the affected area for 20 minutes at a time, several times a day. Be sure to wrap the ice in a towel to protect your skin. It is one of the best sciatica treatment at home.
3. Heat
After the first 72 hours, you can switch to using heat instead of ice. Heat can help to relax muscles and relieve pain and provide immediate relief for sciatica pain. Apply heat to the affected area for 20 minutes at a time, several times a day. You can use a heating pad, hot water bottle, or warm compress. You can easily say goodbye to sciatic nerve pain in just 10 minutes with this natural method.
4. Over-the-counter pain relievers:
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help to reduce pain and inflammation. These are the best medicine for sciatica pain relief immediately. Be sure to follow the directions on the label. Aspadol 100mg tablets is also a pain reliever that your doctor can recommend.
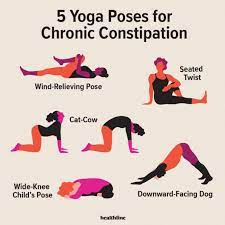
5. Stretching:
Gentle stretching can help to relieve muscle tension and improve flexibility, which can help to reduce sciatica pain. Some helpful immediate relief for sciatica pain stretches include:
- Knee to chest stretch: Lie on your back with your knees bent. Bring one knee up to your chest and hold it there with both hands. Gently pull your knee towards your chest until you feel a stretch in your lower back. Hold for 20 seconds and repeat on the other side.
- Hamstring stretch: Sit on the ground with your legs extended in front of you. Bend forward at the waist, reaching towards your toes. Hold for 20 seconds and repeat 2-3 times.
- Piriformis stretch: Lie on your back with your knees bent and your feet flat on the floor. Cross one ankle over the opposite thigh and gently pull your knee towards your chest. Hold for 20 seconds and repeat on the other side.
Below are some other stretching exercises that you can do:
- Reclining pigeon pose
- Sitting pigeon pose
- Forward pigeon pose
- Knee to the opposite shoulder
- Sitting spinal stretch
- Standing hamstring stretch
- Basic seated stretch
- Standing piriformis stretch
- Groin muscle stretch
- Scissor stretch
6. Exercise:
Regular exercise can help to strengthen the muscles in your back and legs, which can help to prevent future sciatica attacks. Some helpful exercises for sciatica include:
- Core exercises: Core exercises help to strengthen the muscles in your abdomen and back. This can help to improve your posture and reduce stress on your spine and provide immediate relief for sciatica pain. Some examples of core exercises include planks, crunches, and sit-ups.
- Leg exercises: Leg exercises help to strengthen the muscles in your thighs and buttocks. This can help to reduce stress on your lower back. Some examples of leg exercises include squats, lunges, and leg raises. You can easily say goodbye to sciatic nerve pain in just 10 minutes with this natural method.
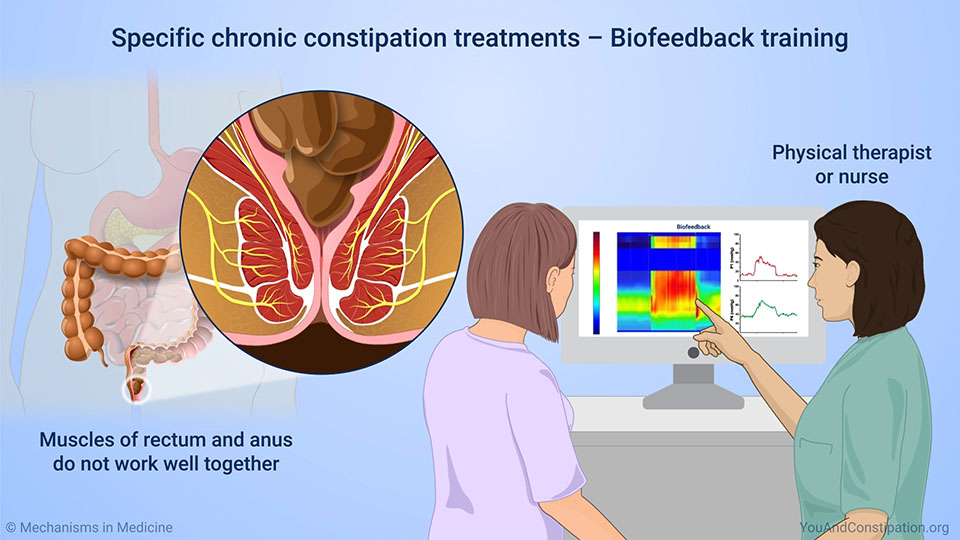
7. Physical therapy:
If other treatments are not effective, or if you want to learn how to manage your sciatica pain on your own, a physical therapist can help. A physical therapist can teach you specific exercises and stretches to help relieve your pain and improve your range of motion. They can also help you to develop a personalized treatment plan that is right for you.
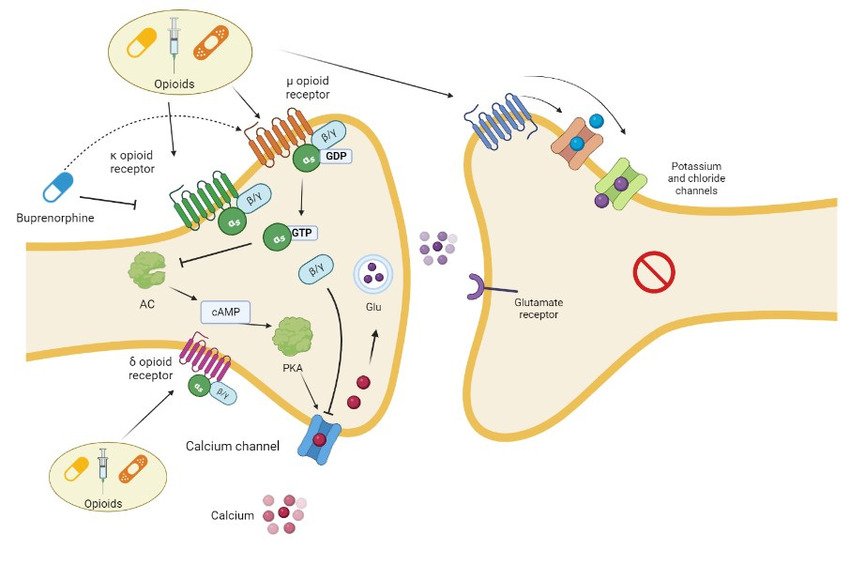
8. Injections:
If other treatments are not effective, your doctor may recommend corticosteroid injections. Corticosteroids are powerful anti-inflammatory drugs that can help to reduce inflammation and pain and offer immediate relief for sciatica pain. However, injections are not a long-term solution, and they may not be effective for everyone.
9. Surgery:
Surgery is rarely necessary for sciatica. However, it may be an option if other treatments have failed and your pain is severe. Surgery can involve removing a herniated disk, widening the spinal canal, or releasing a compressed nerve.
Sciatica pain night guide
Sciatica pain can make it difficult to fall asleep and stay asleep. Here are some tips on how to sleep with sciatica:
Find the best sleeping position for you:
The best sleeping position for sciatica is the one that relieves your pain and allows you to get a good night’s sleep. Some people find relief by sleeping on their side with a pillow between their knees. This helps to keep the spine aligned and reduces pressure on the sciatic nerve. Others find relief by sleeping on their back with a pillow under their knees. This helps to elevate the legs and reduce inflammation.
Use strong painkillers if needed:
If your pain is severe, you may need to take strong painkillers for sciatica, such as prescription medication. However, be sure to talk to your doctor before taking any new medications.
Try sciatic nerve pain relief at night:
There are a number of things you can do to relieve sciatic nerve pain at night, such as:
– Applying a heating pad or ice pack to the affected area
– Taking a warm bath or shower
– Getting a massage
– Stretching your lower back and hamstrings
Here are some additional tips for sleeping with sciatica:
- Create a relaxing bedtime routine: This could include taking a warm bath, reading a book, or listening to calming music.
- Make sure your mattress and pillows are supportive: An old or sagging mattress can worsen sciatica pain. If your mattress is more than 7 years old, it may be time to replace it.
- Avoid caffeine and alcohol before bed: Caffeine and alcohol can interfere with sleep.
- Establish a regular sleep schedule: Go to bed and wake up at the same time each day, even on weekends. This will help to regulate your body’s natural sleep-wake cycle.
How to cure sciatica permanently
While there is no one-size-fits-all answer to this question, there are a number of things you can do to increase your chances of curing sciatica pain permanently.
One of the most important things is to identify and address the underlying cause of your sciatica pain. This may involve losing weight, strengthening your core muscles, or improving your posture. If you have a herniated disk or other spinal condition, you may need surgery to correct the problem.
Once you have addressed the underlying cause of your pain, you can focus on preventing future episodes. This may involve continuing to exercise regularly, maintaining a healthy weight, and practicing good posture. You may also want to avoid activities that aggravate your pain, such as lifting heavy objects or sitting for long periods of time.
If you follow the tips listed above, you can increase your chances of curing sciatica pain permanently. However, it is important to remember that everyone is different, and what works for one person may not work for another. If you are struggling to cure your sciatica pain, talk to your doctor about a personalized treatment plan.
Prevention tips for sciatica pain

- Maintain a healthy weight: Being overweight or obese puts extra stress on your back, which can worsen sciatica pain.
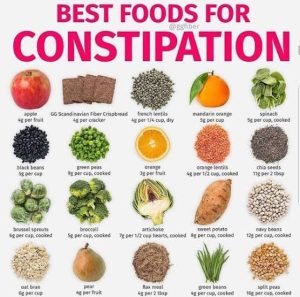
- Eat a healthy diet: Eating a healthy diet can help you maintain a healthy weight and reduce inflammation. Be sure to eat plenty of fruits, vegetables, and whole grains.
- Improve your posture: Good posture helps to keep your spine aligned and reduces stress on your back.
- Avoid sitting or standing for long periods of time: If you have to sit or stand for long periods of time, take breaks to move around and stretch.
- Wear supportive shoes: Supportive shoes can help to improve your posture and reduce stress on your back.
- Get enough sleep: Sleep is essential for healing and recovery. Aim to get 7-8 hours of sleep per night.
- Manage stress: Stress can worsen sciatica pain. Find healthy ways to manage stress, such as exercise, yoga, or meditation, which can also offer immediate relief for sciatica pain.
- See a doctor regularly: If you have chronic sciatica pain, it is important to see a doctor regularly to monitor your condition and make sure that you are getting the appropriate treatment.
When to see a doctor for sciatica pain
Sciatica pain can usually be managed at home with self-care measures, such as rest, ice, heat, and over-the-counter pain relievers. However, there are times when you should see a doctor for sciatica pain, such as if:
- Your pain is severe or does not improve with self-care measures
- Your pain is accompanied by other symptoms, such as numbness, weakness, or tingling in your leg or foot
- You have trouble walking or standing
- You have trouble controlling your bladder or bowels
- You have a history of cancer, diabetes, or other serious medical conditions
- You are pregnant or breastfeeding
If you are experiencing any of the above symptoms, it is important to see a doctor right away to rule out any underlying medical conditions and get the appropriate treatment.
Even if you do not have any of the above symptoms, it is still a good idea to see a doctor if your sciatica pain does not improve after a few weeks of self-care. A doctor can help you to identify the underlying cause of your pain and develop a personalized treatment plan.
Conclusion
Sciatica pain can be a debilitating condition, but it is also preventable and treatable. By following the tips above, you can reduce your risk of developing sciatica pain and manage your symptoms if you do develop it.
If you are experiencing sciatica pain, it is important to see a doctor to rule out any underlying medical conditions and get the appropriate treatment. With proper treatment, most people with sciatica pain make a full recovery.
Remember, you are not alone in this. Millions of people experience sciatica pain every year. There are many resources available to help you manage your pain and get back to your life!
Frequently Asked Questions
1.) How to get rid of sciatica pain in buttocks?
Rest, ice, heat, and over-the-counter pain relievers can help to relieve sciatica pain in the buttocks.
2.) What is the most effective pain relief for sciatica?
Prescription pain relievers and/or injections are the most effective pain relief for sciatica, but should only be used under the supervision of a doctor.
3.) What to do when sciatica pain so bad can’t walk?
If your sciatica pain is so bad that you can’t walk, you should see a doctor immediately.
4.) What helps sciatic nerve pain?
Rest, ice, heat, over-the-counter pain relievers, prescription pain relievers, injections, physical therapy, and surgery can all help to relieve sciatic nerve pain.
5.) How can I relieve sciatica pain fast?
Over-the-counter pain relievers, ice, and heat can provide fast relief for sciatica pain.
6.) What is the best painkiller for sciatica?
Prescription pain relievers are the most effective painkillers for sciatica, but should only be used under the supervision of a doctor.
7.) Is there any home remedy for sciatica?
Yes, rest, ice, heat, and exercise are all home remedies that can help relieve sciatica pain. You can say goodbye to sciatic nerve pain in just 10 minutes with this natural method!
8.) What are the top 3 exercises for sciatica?
The top 3 exercises for sciatica are the knee-to-chest stretch, the hamstring stretch, and the piriformis stretch, which can provide sciatica relief in 8 minutes approximately.
9.) How do you sleep with sciatica?
Sleeping on your side with a pillow between your knees or sleeping on your back with a pillow under your knees may help relieve sciatica pain while you sleep.
10.) What is the main cause of sciatica?
The main cause of sciatica is a herniated disk, which puts pressure on the sciatic nerve.
11.) Why is sciatica worse at night?
Sciatica pain may be worse at night because inflammation tends to increase at night.
12.) What foods should you avoid with sciatica?
There is no specific diet that is recommended for people with sciatica. However, it is generally recommended to eat a healthy diet that is low in processed foods and high in fruits, vegetables, and whole grains.